Osteoporosis in Women
Keeping your bones healthy and strong:
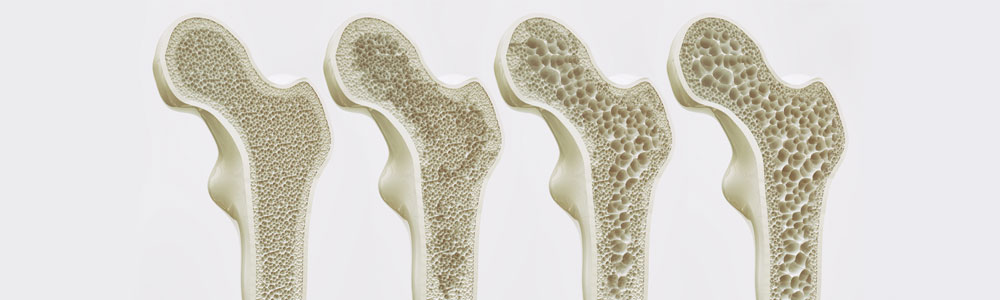
In osteoporosis, the inside of the bones becomes porous and thin. Over time this weakens the bones and may make them more likely to break.
Osteoporosis is much more common in women then in men. This is because women have less bone mass then men. Women need the female hormone estrogen to keep their bones strong. Men, if they live long enough are also at risk of getting osteoporosis later in life.
Once total bone mass has peaked –around 35 – all adults start to lose it. In women, the rate of bone lose speeds up during menopause, when estrogen levels fall. Bone loss may also occur if both ovaries are removed by surgery. Your ovaries make estrogen.
You may not know that you have osteoporosis until you have serious signs. Signs include a broken wrist or hip, low back pain or a hunched back. You may get shorter over time. This is because osteoporosis can cause the bones in your spine, vertebrae, to collapse. These are called compression fractures, and they can cause sever back pain. These problems can occur after a lot of bone calcium has been lost.
Below is a list of things that can put you at risk for osteoporosis. The more of these that apply to you, the higher your risk. Talk to your family doctor if you think that you may be at risk for osteoporosis.
- Menopause before age 48
- Surgery to remove ovaries before normal menopause
- Not getting enough exercise
- Smoking
- Osteoporosis in your family
- Alcohol abuse
- Small bone frame
- Thin
- Fair skin
- Hyperthyroidism
- Use of steroids
Hormone replacement therapy is one of the best ways to keep osteoporosis form getting worse once it has started. If you begin hormone replacement therapy at the time of menopause, it can help prevent osteoporosis form happening at all.
In replacement therapy, you take hormones, such as estrogen and progestin, that your body stops making at menopause or if your ovaries are replaced by surgery.
Estrogen keeps your bones from losing calcium and can help your bones stay strong. Broken bones, a loss in height and other signs of osteoporosis can all be prevented.
Taking estrogen will also treats signs of menopause, such as hot flashes and vaginal dryness. It may also help protect you against heart disease and reduce the risk of ovarian cancer. If the hormone progestin is taken with estrogen, hormone treatment may also decrease your risk of endomentrial cancer (cancer of the lining of the uterus).
Side effects of estrogen may include sore breasts, the return of menstrual periods, slight bleeding between periods, weight gain, and gallstones. The risk of breast cancer may or may not be increased. Your breasts may get lumpy.
If you take estrogen without progestin, you may be at greater risk of endomentrial cancer. Progestin offsets the risk. This is why your doctor may prescribe Progestin for you (if you have not had your uterus removed).
Your doctor may want you to have a mammogram to watch for changes in your breasts. Pap smears, which are use to test for signs of cancer in your cervix (the opening of the uterus), should be done every year.
Some doctors also check the lining of the uterus for cancer with a procedure called endomentrial sampling. During this test, a sample from inside your uterus is taken with a very thin instrument. The sample is checked under a microscope to make sure there are no abnormal cells. Your doctor may do this before starting you on hormone replacement therapy or if you have unusual bleeding from your vagina while in therapy.
Hormones can be started during menopause or at any time after menopause. Your doctor may also start you on them if you have had surgery to remove your ovaries. It’s usually best to start hormone treatment as soon as possible. You’ll get the most benefit if you start taking hormones within a year after menopause.
As soon as you stop hormone replacement therapy, your bones start to lose calcium. Symptoms of menopause also return. The longer you take replacement therapy, the less likely you will get osteoporosis. What is Calcitonin? Calcitonin is a hormone that helps prevent further bone loss in people that have osteoporosis. It also helps reduce the pain some people have with osteoporosis. Calcitonin can be taken as a shot every day or as a nasal spray. A common side effect is nausea.
Alendronata is a non hormonal treatment for osteoporosis. Alendronata helps reduce the risk of hip and spine fractures by decreasing the rate of bone loss. Since it is not a hormone, alendronata may be suitable for men and for women who have a personal or family history of breast cancer. Alendronata, like calcitonin, however, does not offer the additional protective effects of estrogen. The most common side effect is upset stomach.
Women need about 1000mg of calcium a day before menopause. The same amount is needed after menopause if you are on estrogen. Up to 1500mg of calcium is needed a day after menopause if you are not taking estrogen.
It is usually best to try to get the calcium you need from food. Sometimes, women to do not eat enough dairy products because they think these foods are to fattening. But, nonfat and low-fat dairy products have as much calcium as those made from whole milk. Other sources of calcium include dried beans, sardines, and broccoli.
About 300mg of calcium is provided in each of the following foods: 1 cup of milk or yogurt, two cups of broccoli, or six to seven sardines.
Your doctor may suggest taking a calcium pill if you do not get enough calcium from the food you eat. Take it at mealtime or with a sip of milk. Vitamin D and lactose (the natural sugar in milk) help to absorb the calcium.
TIPS TO KEEP BONES STRONG AND AVOID FALLS.
- Exercise.
- Eat a normal, well-balanced diet.
- Don’t use throw rugs in your home. They can trip you.
- Wear flat, rubber-soled shoes.
- Use a cane or walker if you need to.
- Put hand grips and safety mats in your bathtub or shower.
- Be sure stairways are well lit.
- Don’t stoop to pick things up. Pick up things by pending your knees and keeping your back straight.
- Quit smoking. Smoking makes osteoporosis worse and may cancel out the benefits of estrogen replacement therapy.
This information provides a general overview on osteoporosis and may not apply to everyone. Talk to your family doctor to find out if this information applies to you and to get more information on this subject.